COVID-19 positive – How to use a pulse oximeter in children
IMPORTANT : The following information has been supplied by The Health Navigator New Zealand website - a trusted source of information. Asthma NZ recommend this advice is wise advice for those in our community who have respiratory conditions and if in doubt at all, speak with an Asthma NZ nurse for further advice around managing a respiratory condition. If at any time your child has trouble breathing, or their symptoms become suddenly worse, call 111 for an ambulance.

What is an oximeter?
A pulse oximeter is a small device that clips on to your child's finger. It quickly and easily checks your child's oxygen levels. This guide (developed with KidsHealth NZ) will explain how to use a pulse oximeter, what the numbers mean and what actions you should take.
Note: The information on this page is for the use of a pulse oximeter in children. For use in adults, see how to use a pulse oximeter in adults.
What does a pulse oximeter measure?
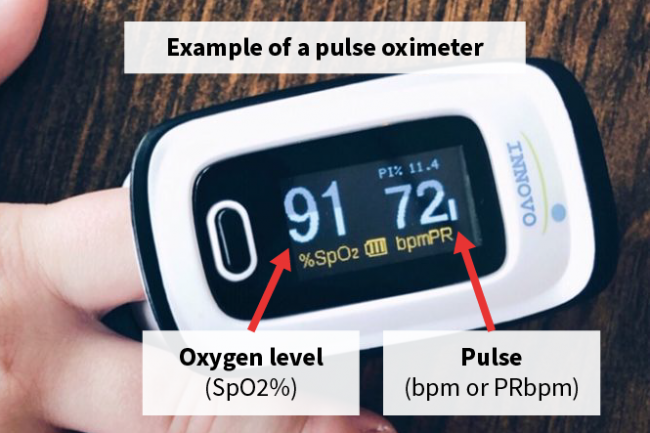
A pulse oximeter measures 2 things — pulse and oxygen saturation level.
Pulse
This is a measure of how fast your child's heart is beating. Your child's pulse is measured in beats per minute (bpm). On your child's pulse oximeter this number may show as bpm or PRbpm (pulse rate/beats per minute).
Oxygen saturation level
This is a measure of how much oxygen is in your child's blood. Your child's oxygen saturation is measured as a percentage (scored out of 100). On your child's pulse oximeter this number may show as SpO2% (saturation percentage of oxygen).
If at any time your child has trouble breathing, or their symptoms become suddenly worse, call 111 for an ambulance.
What pulse oximeter do I use for my child?
Children over 30kg (10 years or older if you don’t know your child’s weight)
You can use an adult pulse oximeter for your child, as long as their finger goes all the way to the end of the probe. Using an adult oximeter on smaller children may give an inaccurate reading.
Children under 30 kg (9 years or younger if you don’t know your child’s weight)
Children under 30kg need a child's pulse oximeter. This may be either an oximeter that:
- clips onto the finger with a child sized clip
- wraps around the finger with tape.
How do I use a pulse oximeter?
There are different brands of these devices. Please read the manufacturer's instructions. The following is a general guide. If you have any questions, ask your healthcare team.
Preparing
- Wash your child's hands.
- Make sure they don't have nail polish or glitter on - the light beams in the sensor measure through your child's fingernail.
- Make sure your child has been resting for at least 5 minutes before taking the reading.
- If your child's hands are cold, warm them by rubbing them together.
- Rest your child's arm and hand and keep them still while taking the reading.
- Their hand should be at waist level - try resting their hand on a table or the arm of a chair.
Taking the reading
- Switch the pulse oximeter ON and the display will light up.
- If using a pulse oximeter with a clip, squeeze to open and put your child's finger in until their fingertip touches the end.
- If using a pulse oximeter with tape, make sure the two surfaces are on opposite sides of the finger and keep them in place by wrapping the tape around.
- It works best on the middle or index finger of either hand.
- Keep your child's hand still and wait for 1 to 2 minutes until their pulse (bpm/PRbpm) is steady and their oxygen saturation (SpO2%) number has not changed for at least 5 seconds.
- If the numbers are not steady, try a different finger.
Recording the numbers
- Record the oxygen saturation number ‘SpO2%’ and the pulse rate number ‘PRbpm’ in your child's pulse oximeter and symptom diary.
- Your child's heart rate and oxygen level numbers are easy to mix up - be careful to record these correctly.
- Measure and record your child's pulse (heart rate) and oxygen level 3 times a day at about the same time every day.
- These numbers will help your child's healthcare team monitor your child safely at home.
- Take extra measurements if you notice a change in your child's health.
- To clean your device, check the manufacturer’s instructions.
What do pulse oximeter numbers mean?
The following is a general guide for children who usually have normal saturation levels.
| Oxygen saturation SpO2% |
Action |
| 95–99 | ✔ Acceptable |
| 92–94 | Call your healthcare team |
| Below 92 | Call 111 for urgent medical care |
Your healthcare team may give you specific advice about what action to take for your child at different oxygen saturation levels. For example, if your child normally has low saturation levels because of congenital heart disease, the advice may be:
- a drop of 3% or more from their usual level — call your healthcare team
- a drop of 6% or more from their usual level — call 111.
Are there other signs or symptoms of low oxygen levels?
A pulse oximeter is a small device that clips on to your child's finger. It quickly and easily checks your child's oxygen levels. This guide (developed with KidsHealth NZ) will explain how to use a pulse oximeter, what the numbers mean and what actions you should take.
Note: The information on this page is for the use of a pulse oximeter in children. For use in adults, see how to use a pulse oximeter in adults.
What is a pulse oximeter?
A pulse oximeter is a small device that clips on to your child's finger. It quickly and easily checks your child's oxygen levels. It uses light beams in a sensor to estimate the amount of oxygen in your child's blood, without taking a blood sample. This helps to track how well your child's lungs are working.
What does a pulse oximeter measure?
A pulse oximeter measures 2 things — pulse and oxygen saturation level.
Pulse
This is a measure of how fast your child's heart is beating. Your child's pulse is measured in beats per minute (bpm). On your child's pulse oximeter this number may show as bpm or PRbpm (pulse rate/beats per minute).
Oxygen saturation level
This is a measure of how much oxygen is in your child's blood. Your child's oxygen saturation is measured as a percentage (scored out of 100). On your child's pulse oximeter this number may show as SpO2% (saturation percentage of oxygen).
|
If at any time your child has trouble breathing, or their symptoms become suddenly worse, call 111 for an ambulance. |
| Check the signs that show your baby or child might be struggling to breathe. |
What pulse oximeter do I use for my child?
Children over 30kg (10 years or older if you don’t know your child’s weight)
You can use an adult pulse oximeter for your child, as long as their finger goes all the way to the end of the probe. Using an adult oximeter on smaller children may give an inaccurate reading.
Children under 30 kg (9 years or younger if you don’t know your child’s weight)
Children under 30kg need a child's pulse oximeter. This may be either an oximeter that:
- clips onto the finger with a child sized clip
- wraps around the finger with tape.
How do I use a pulse oximeter?
There are different brands of these devices. Please read the manufacturer's instructions. The following is a general guide. If you have any questions, ask your healthcare team.
Preparing
- Wash your child's hands.
- Make sure they don't have nail polish or glitter on - the light beams in the sensor measure through your child's fingernail.
- Make sure your child has been resting for at least 5 minutes before taking the reading.
- If your child's hands are cold, warm them by rubbing them together.
- Rest your child's arm and hand and keep them still while taking the reading.
- Their hand should be at waist level - try resting their hand on a table or the arm of a chair.
Taking the reading
- Switch the pulse oximeter ON and the display will light up.
- If using a pulse oximeter with a clip, squeeze to open and put your child's finger in until their fingertip touches the end.
- If using a pulse oximeter with tape, make sure the two surfaces are on opposite sides of the finger and keep them in place by wrapping the tape around.
- It works best on the middle or index finger of either hand.
- Keep your child's hand still and wait for 1 to 2 minutes until their pulse (bpm/PRbpm) is steady and their oxygen saturation (SpO2%) number has not changed for at least 5 seconds.
- If the numbers are not steady, try a different finger.
Recording the numbers
- Record the oxygen saturation number ‘SpO2%’ and the pulse rate number ‘PRbpm’ in your child's pulse oximeter and symptom diary.
- Your child's heart rate and oxygen level numbers are easy to mix up - be careful to record these correctly.
- Measure and record your child's pulse (heart rate) and oxygen level 3 times a day at about the same time every day.
- These numbers will help your child's healthcare team monitor your child safely at home.
- Take extra measurements if you notice a change in your child's health.
- To clean your device, check the manufacturer’s instructions.
What do pulse oximeter numbers mean?
The following is a general guide for children who usually have normal saturation levels.
| Oxygen saturation SpO2% |
Action |
| 95–99 | ✔ Acceptable |
| 92–94 | Call your healthcare team |
| Below 92 | Call 111 for urgent medical care |
Your healthcare team may give you specific advice about what action to take for your child at different oxygen saturation levels. For example, if your child normally has low saturation levels because of congenital heart disease, the advice may be:
- a drop of 3% or more from their usual level — call your healthcare team
- a drop of 6% or more from their usual level — call 111.
Are there other signs or symptoms of low oxygen levels?
Don't rely only on a pulse oximeter to assess your child's health condition or oxygen level. It is only a measurement device.
Other signs or symptoms of low oxygen levels can be if your child:
- has blue lips and tongue
- has severe difficulty breathing
- has episodes of irregular breathing or stopping breathing
- is unconscious, or you can't wake them up properly.
Check the signs that show your baby or child might be struggling to breathe. If you have any concerns or questions, contact your child's healthcare team directly.
| Credits | |
|
Content courtesy of KidsHealth NZ which has been created by a partnership between the Paediatric Society of New Zealand (PSNZ) and the Starship Foundation, supported and funded by the Ministry of Health. |



